Abstract
Background:
Venous and arterial thromboembolism (VTE/ATE) in patients with cancer are a significant cause of morbidity and mortality. Platinum-based chemotherapy (Platinum) has been associated with increased risk of VTE and ATE. In the last decade immunotherapy (IO) has emerged as first line treatment for many patients, alone or in combination with Platinum. Immune checkpoint inhibition can lead to a systemic proinflammatory state with some suggesting an associated procoagulant effect. A systematic review of studies on IO in advanced cancer reported incidence of 2.7% VTE and 1.1% ATE (n=20,273, Solinas et al 2020), concluding ATE/VTE is relatively rare with IO. However, emerging real world data suggest a higher incidence of thrombosis than initially reported, and how VTE/ATE incidence compares with IO as compared with Platinum remains unknown.
Methods:
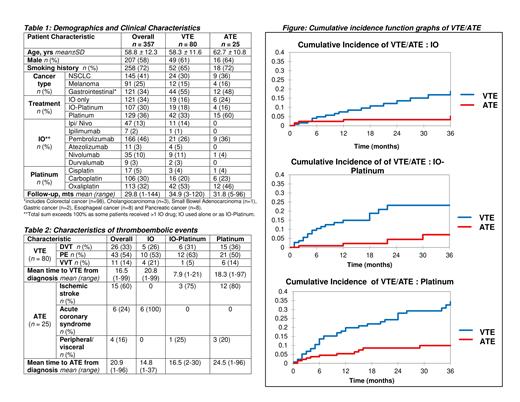
We conducted a retrospective cohort study of consecutive patients with advanced solid tumors including non-small cell lung cancer (NSCLC, unresectable Stage III or Stage IV), melanoma (Stage III or Stage IV) and gastrointestinal cancers (Stage IV) during the period 2014-2020 at the Brown Cancer Center. Patients with thrombophilia, anticoagulation use, >1 malignancy, and use of regimens without IO/Platinum were excluded. Treatments included IO, Platinum (cisplatin, carboplatin, oxaliplatin) or combined IO-Platinum. VTE was defined as deep vein thrombosis, pulmonary embolism or visceral vein thrombosis. ATE was defined as any arterial thromboembolic event including arterial stroke, myocardial infarction, peripheral arterial thrombosis and visceral arterial thromboses. The primary outcomes of the study were cumulative incidence rates of VTE and ATE with events recorded in time from diagnosis. Cumulative incidence analyses were performed to compare rates of VTE and ATE for the different modalities of treatment (IO, IO-Platinum, Platinum).
Results:
A total of 357 patients were included. Clinical characteristics are presented in Table 1 - just over half were male, median age 59 yrs and predominant history of smoking. NSCLC was most represented (41%) followed by GI cancer (34%) and melanoma (25%). Treatment modalities were fairly distributed : IO (34%), IO-Platinum (30%) and Platinum (36%). Over a median follow up of 2.5 yrs, VTE occurred in 80 patients (22%), most commonly PE followed by DVT and VVT (Table 2). At median follow up, the cumulative incidence of VTE with IO was 15.1% [95% CI (9.3-24.6)] vs. IO-Platinum at 23.2% [95% CI (15.1-35.7)] and Platinum at 29.2% [95% CI (21.7-39.4)]. ATE occurred in 25 patients overall (7%) (Table 2). At median follow up, cumulative incidence of ATE with IO was 3.3% [95% CI (1.3-8.7)] vs. IO-Platinum at 7.0% [95% CI (2.5-19.4)] and Platinum at 9.9% [95% CI (5.6-17.6)]. Cumulative incidence frequencies for VTE/ATE are presented graphically according to each treatment modality (Figure).
Conclusion:
In this cohort of patients, increased incidence of VTE/ATE over time was seen following immunotherapy alone or combined with platinum-based chemotherapy. Immunotherapy can induce a durable response with unprecedented survival benefits and patients with advanced solid tumors are at risk for increasingly longer periods. The reasons behind increased real world incidence relative to historical adverse event reporting are likely multifactorial and further research in larger cohorts is needed.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal